Bone health plays a critical role in long-term well-being, yet it is often overlooked until a problem arises. Conditions such as osteopenia and osteoporosis can develop gradually over many years without obvious symptoms, meaning bone loss is frequently undetected until a fracture occurs. This is why understanding bone health and monitoring changes early is so important.
DEXA scans are widely recognised as the gold standard for assessing bone health. Through Bone Mineral Density (BMD) testing, DEXA provides an objective measure of bone strength and fracture risk, allowing clinicians to identify changes long before symptoms appear. When interpreted correctly, these results can help guide informed decisions around lifestyle, exercise and ongoing monitoring.
This article explains how DEXA scans are used in the assessment of osteoporosis, what bone density results mean, and how bone health can be monitored over time. It also explores practical steps that support bone health following a DEXA scan, helping you understand how this information fits into a proactive, long-term approach to skeletal wellbeing.
Key Takeaways
- Osteoporosis often develops without symptoms, making early monitoring essential
- DEXA scans are the gold standard for measuring Bone Mineral Density (BMD)
- Bone Mineral Density is different from bone mass measured in body composition scans
- T-scores and Z-scores help classify bone health and fracture risk
- Bone density changes slowly, making long-term tracking more meaningful than single scans
- Lifestyle, exercise and nutrition play an important role in supporting bone health
- Understanding results helps guide informed, proactive bone health decisions
Summary Table: DEXA Scans and Bone Health
| Aspect | What It Shows | Why It Matters |
| Bone Mineral Density (BMD) | Measure of bone strength and density | Assesses osteoporosis and fracture risk |
| T-score | Comparison to young adult reference | Used to classify normal bone, osteopenia or osteoporosis |
| Z-score | Comparison to age-matched population | Helps identify bone loss outside expected ranges |
| DEXA technology | Dual-energy X-ray imaging | Provides accurate, repeatable bone assessment |
| Monitoring over time | Changes in bone density | Tracks progression or stability of bone health |
| Radiation exposure | Very low dose | Safe for appropriate repeat assessments |
What Is Osteoporosis and How Does It Develop?
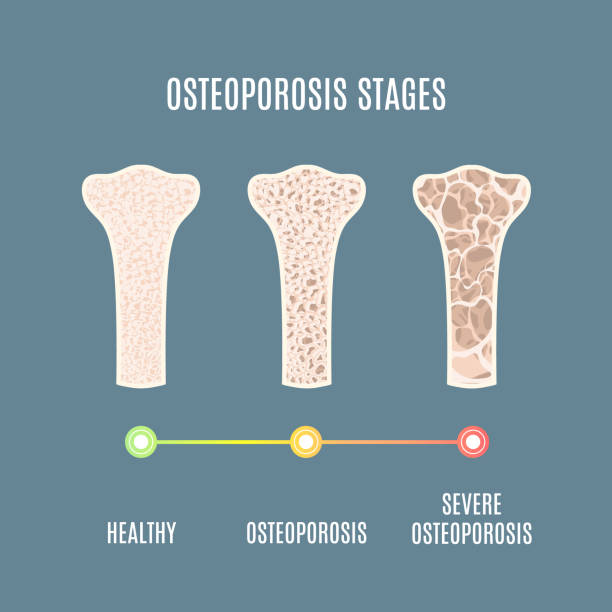
Osteoporosis is a condition characterised by a reduction in bone strength, making bones more fragile and more susceptible to fractures. It develops when bone breakdown occurs faster than new bone is formed, leading to a gradual loss of bone density over time. A related condition, osteopenia, refers to lower-than-normal bone density that has not yet reached the threshold for osteoporosis.
Bone is living tissue that is constantly being remodelled. In younger years, bone formation typically exceeds bone breakdown, allowing bones to become stronger and denser. As people age, this balance shifts. Bone breakdown begins to outpace bone formation, resulting in a gradual decline in bone density. This process can accelerate due to hormonal changes, particularly during and after menopause.
Osteoporosis often develops without noticeable symptoms. Many individuals are unaware of changes in their bone health until a fracture occurs, sometimes from a minor fall or everyday movement. This is why osteoporosis is sometimes referred to as a “silent” condition.
Several factors can increase the risk of developing osteoporosis, including age, family history, hormonal changes, low body weight, inadequate nutrition, limited weight-bearing activity and certain medications. Understanding how osteoporosis develops highlights the importance of early assessment and ongoing monitoring through tools such as DEXA scans.
How DEXA Scans Are Used to Assess Bone Health

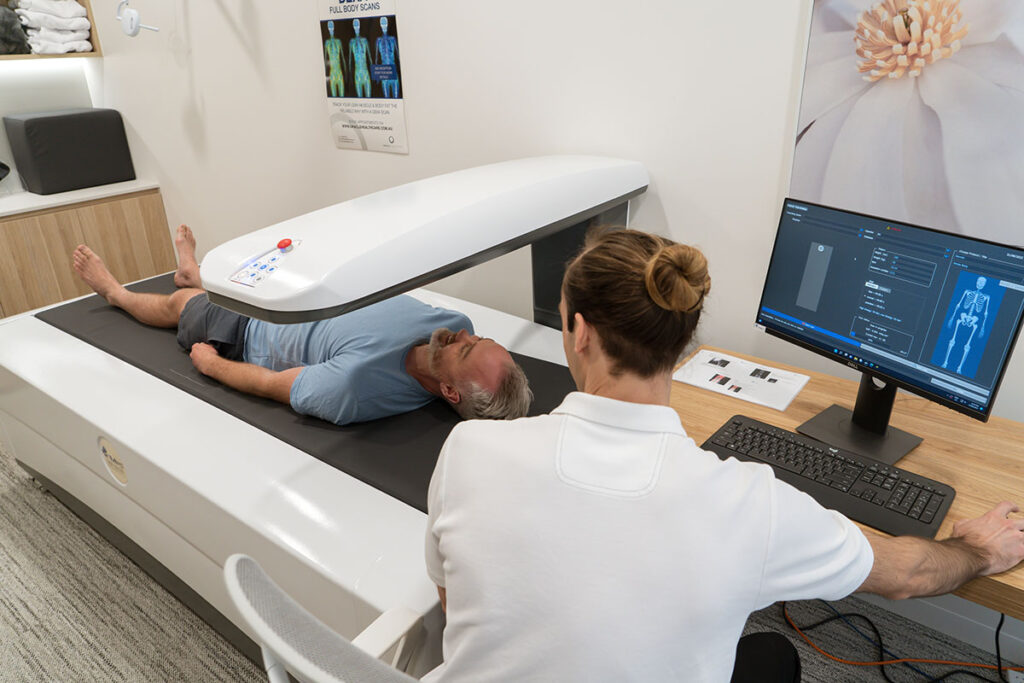
DEXA scans play a central role in the assessment and monitoring of bone health through Bone Mineral Density (BMD) testing. A BMD DEXA scan measures how dense and mineralised the bones are, providing an objective indicator of bone strength and fracture risk.
It is important to distinguish between a DEXA body composition scan and a DEXA Bone Mineral Density exam. While both use the same underlying imaging technology and are performed on the same type of machine, they are separate assessments with different purposes. A body composition scan measures bone mass as part of overall tissue distribution, whereas a BMD exam specifically evaluates bone density using dedicated medical software and protocols.
During a BMD exam, specific skeletal sites such as the spine and hip are analysed, as these areas are most predictive of fracture risk. The results are interpreted using standardised scoring systems and are reported by a Radiologist, ensuring clinical accuracy and consistency. This medical reporting is what allows BMD DEXA scans to be used in the diagnosis and monitoring of conditions such as osteopenia and osteoporosis.
Because DEXA provides precise and repeatable measurements, it is well suited to tracking changes in bone density over time. When used appropriately, DEXA scanning enables early identification of bone loss and supports informed decisions around monitoring and long-term bone health management.
Understanding T-Scores and Z-Scores
When a Bone Mineral Density (BMD) DEXA scan is performed, results are reported using T-scores and Z-scores. These scores help place an individual’s bone density into context and are used to assess bone health and fracture risk.
A T-score compares your bone density to that of a healthy young adult of the same sex. This comparison is used to classify bone health into standard categories. A T-score of –1.0 or above is considered normal bone density. Scores between –1.0 and –2.5 indicate osteopenia, while a T-score of –2.5 or lower is used to diagnose osteoporosis. These thresholds are widely accepted and help clinicians assess fracture risk.
A Z-score compares your bone density to what is expected for someone of the same age, sex and body size. Z-scores are particularly useful for identifying whether bone loss is occurring earlier or more rapidly than expected. While Z-scores are not used to diagnose osteoporosis, they provide valuable context, especially for younger individuals or those with additional risk factors.
It is important to interpret T-scores and Z-scores alongside clinical history, lifestyle factors and previous scan results. Bone density changes gradually, and a single score does not tell the whole story. Understanding how these scores work helps place DEXA results into a broader and more meaningful health context.
Who Should Consider a DEXA Scan for Osteoporosis?
A DEXA scan for osteoporosis assessment may be appropriate for individuals who have risk factors for reduced bone density or who want to proactively monitor their bone health. Because osteoporosis often develops without symptoms, screening decisions are usually based on risk rather than how a person feels.
Post-menopausal women are one of the groups most commonly recommended for bone density assessment. Hormonal changes after menopause can accelerate bone loss, making early monitoring important even in the absence of symptoms.
Adults over the age of 50, particularly those with additional risk factors, may also benefit from a DEXA scan. Age-related bone loss is gradual, and identifying changes early allows for more informed long-term management.
Individuals with a family history of osteoporosis or fractures, those who have experienced a low-impact fracture, or people who have used long-term corticosteroid medications may also be advised to consider bone density testing. Low body weight, limited weight-bearing activity and certain medical conditions can further increase risk.
For some people, a DEXA scan is part of proactive health monitoring rather than a response to a specific concern. Understanding whether and when a scan is appropriate is best guided by individual risk factors and professional advice.
Monitoring Bone Health Over Time with DEXA
Bone density changes gradually, which means monitoring bone health is best approached as a long-term process rather than a one-off assessment. DEXA scans are particularly well suited to this role because they provide precise and repeatable measurements that allow changes to be tracked reliably over time.
When monitoring bone health, trends are more informative than individual results. Small variations between scans are normal and do not necessarily indicate meaningful change. For this reason, repeat DEXA scans are typically spaced months or years apart, depending on individual risk factors, baseline results and clinical guidance.
Consistency is important when comparing scans. Using the same type of scan, similar positioning and comparable testing conditions helps ensure that changes reflect real differences in bone density rather than measurement variability. This consistency allows clinicians to assess whether bone density is stable, declining or improving over time.
By tracking bone density longitudinally, DEXA scans support informed decision-making around lifestyle adjustments, exercise strategies and ongoing monitoring. This approach helps individuals and healthcare professionals respond to changes early and maintain a proactive focus on long-term bone health.
Can You Improve Bone Health After a DEXA Scan?
A DEXA scan provides valuable insight into bone health, but it is only the starting point. While bone density changes slowly, there are well-established lifestyle factors that play an important role in supporting bone strength over time.
Weight-bearing and resistance exercise are among the most effective ways to stimulate bone maintenance. Activities that place controlled stress on bones, such as walking, strength training and impact-appropriate exercises, encourage the body to preserve bone density. Exercise programs should be tailored to individual ability and risk level, particularly for those with reduced bone density.
Nutrition also plays a key role. Adequate intake of calcium, protein and vitamin D supports bone structure and mineralisation. Energy availability is equally important, as chronic under-fueling can negatively affect bone health, particularly in older adults.
Lifestyle factors such as smoking, excessive alcohol intake and prolonged inactivity can contribute to bone loss over time. Addressing these factors, where relevant, can help support long-term skeletal health.
Importantly, changes in bone density are gradual. Improvements or stabilisation are typically assessed over extended periods rather than between short-term scans. DEXA results can help guide informed discussions and support a proactive, long-term approach to maintaining bone health rather than expecting rapid change.
DEXA Scans, Medicare and Private Testing in Australia
In Australia, access to DEXA scans for bone health depends on the purpose of the scan and individual eligibility criteria. Medicare provides rebates for Bone Mineral Density (BMD) DEXA scans only when specific clinical conditions are met. These may include monitoring osteoporosis, assessing fracture risk or managing certain medical conditions, and typically require a referral from a GP or specialist.
Not all individuals will meet the criteria for a Medicare-rebated scan. In these cases, private BMD DEXA scans may be used for assessment or monitoring. Private scans do not require Medicare eligibility and may still involve a referral depending on the provider and purpose of the test.
It is also important to distinguish between medical BMD scans and DEXA body composition scans. Body composition scans are not covered by Medicare and are used for monitoring fat mass, lean mass and bone mass rather than diagnosing osteoporosis. These scans are typically booked directly and paid for privately.
Understanding the difference between medical and private testing helps set appropriate expectations around access, referrals and reporting. Regardless of funding pathway, DEXA scanning remains a reliable tool for assessing and monitoring bone health when used appropriately.
Common Misunderstandings About Osteoporosis and DEXA
One of the most common misunderstandings about osteoporosis is the belief that symptoms will appear early. In reality, bone loss often progresses silently, and many people are unaware of changes in their bone density until a fracture occurs. This is why proactive assessment and monitoring are important for those at risk.
Another frequent source of confusion is the difference between bone mass and Bone Mineral Density (BMD). A DEXA body composition scan measures bone mass as part of overall tissue distribution, while a BMD exam is a separate medical assessment used to evaluate bone strength and fracture risk. Understanding this distinction helps avoid misinterpretation of results.
Some people also expect rapid improvements in bone density following lifestyle changes. Bone adapts slowly, and meaningful changes typically occur over extended periods rather than between short-term scans. Comparing results from a single scan or against other people’s results can also lead to unnecessary concern.
DEXA results are most useful when interpreted in context, alongside clinical history, risk factors and long-term trends. A clear understanding of what DEXA can and cannot show helps ensure results are used appropriately and constructively.
Using DEXA Results to Support Long-Term Bone Health
DEXA results are most valuable when used as part of a long-term approach to bone health rather than as a one-off measurement. By understanding Bone Mineral Density results and how they change over time, individuals can make informed decisions about lifestyle, exercise and ongoing monitoring.
DEXA scans help establish a clear baseline, allowing future scans to be compared meaningfully. This makes it easier to identify whether bone density is stable, declining or responding positively to supportive lifestyle changes. When used alongside professional guidance, DEXA data can inform appropriate adjustments without relying on guesswork.
Importantly, DEXA results should always be interpreted in context. Factors such as age, medical history, activity levels and nutrition all influence bone health. Rather than focusing on a single score, using DEXA to monitor trends supports a more balanced and proactive approach to maintaining skeletal strength over time.
By providing objective, repeatable data, DEXA scans help shift bone health management from reactive to informed and preventative, supporting long-term confidence and clarity.
Final Thoughts
Osteoporosis and reduced bone density often develop gradually and without symptoms, making early understanding and monitoring essential. DEXA scans provide a reliable and clinically validated way to assess bone health through Bone Mineral Density testing, offering insight long before fractures or complications occur.
When interpreted correctly, DEXA results support informed decisions around lifestyle, monitoring and long-term bone health strategies. By focusing on trends rather than isolated numbers, individuals can take a proactive approach to maintaining bone strength and reducing future risk.
Understanding how DEXA scans are used in osteoporosis assessment empowers people to engage more confidently with their bone health and make choices that support long-term wellbeing.
FAQs Answered
Where can I get a DEXA scan for osteoporosis in Sydney?
In Sydney, DEXA scans for osteoporosis assessment are available through medical imaging centres and specialised clinics that offer Bone Mineral Density (BMD) DEXA scans. These scans are performed using medical-grade DEXA equipment and are reported by a Radiologist. Access may be through Medicare-rebated pathways if eligibility criteria are met, or privately if not.
What is the best DEXA scan for osteoporosis assessment?
The best DEXA scan for osteoporosis assessment is a Bone Mineral Density (BMD) DEXA scan. This type of scan focuses on clinically relevant skeletal sites, such as the spine and hip, and uses dedicated medical software to assess bone density and fracture risk. Body composition DEXA scans measure bone mass, not bone density, and are not used to diagnose osteoporosis.
Is a DEXA scan the most accurate test for osteoporosis?
Yes. DEXA scanning is widely recognised as the gold standard for assessing osteoporosis risk. Bone Mineral Density DEXA scans provide accurate, repeatable measurements of bone density and are used internationally in clinical guidelines for diagnosing and monitoring osteoporosis.
Do I need a referral for a DEXA scan for osteoporosis?
A referral from a GP or specialist is required for Medicare-rebated Bone Mineral Density DEXA scans, as eligibility depends on specific clinical criteria. For private BMD DEXA scans, referral requirements may vary by provider, but a referral is often still requested to ensure appropriate assessment and reporting.
How often should you get a DEXA scan to monitor osteoporosis?
Bone density changes slowly, so DEXA scans for osteoporosis monitoring are commonly repeated every 1 to 2 years. The appropriate interval depends on baseline results, risk factors and clinical guidance. Monitoring trends over time is more meaningful than frequent short-term testing.
What do DEXA scan results show for osteoporosis risk?
DEXA scan results report Bone Mineral Density using T-scores and Z-scores. These scores indicate whether bone density is within the normal range, reduced (osteopenia) or consistent with osteoporosis. Results are used to assess fracture risk and guide long-term monitoring decisions.
Is a DEXA scan safe for repeated bone density testing?
Yes. DEXA scans use a very low dose of radiation, comparable to natural background radiation experienced in daily life. This low exposure makes DEXA suitable for repeated use when clinically appropriate, such as long-term osteoporosis monitoring.
“