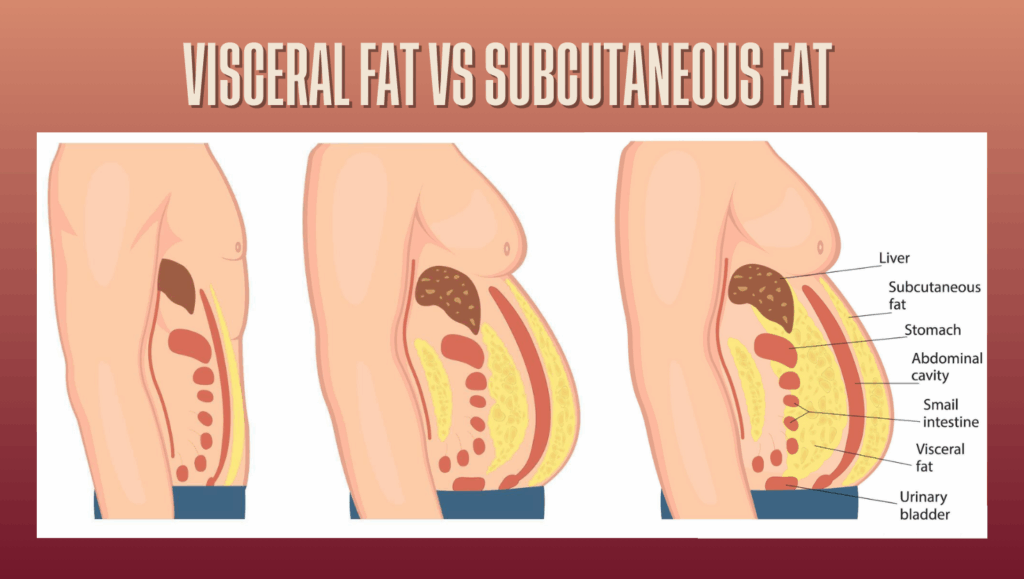
Not all body fat carries the same health risk. While subcutaneous fat sits beneath the skin and is often the focus of aesthetic goals, visceral fat is stored deep within the abdominal cavity, surrounding vital organs such as the liver, pancreas and intestines. This type of fat is far less visible, yet far more closely linked to long-term health complications.
Many people assume that if they look lean or maintain a healthy body weight, their health risk is low. However, visceral fat does not always correlate with appearance or scale weight. Individuals who appear fit or fall within a normal BMI range can still carry elevated levels of visceral fat, placing them at increased risk of metabolic and cardiovascular conditions.
The challenge is that visceral fat cannot be accurately assessed using traditional methods such as body weight, BMI, tape measurements or skinfolds. These tools focus on external or estimated markers and fail to detect internal fat storage. This is where DEXA body composition scanning plays a critical role.
DEXA is one of the few non-invasive methods capable of objectively estimating visceral fat. By analysing the abdominal region using dual-energy X-ray technology, it provides clear insight into internal fat levels and how they change over time. This article explains what visceral fat is, why it matters, and how DEXA scans can be used to identify and monitor this often-overlooked health risk.
Key Takeaways
- Visceral fat is stored around internal organs and is linked to serious health risks
- You cannot reliably assess visceral fat through weight, BMI or appearance
- People with normal weight can still have high visceral fat levels
- DEXA provides an objective, non-invasive estimate of visceral fat
- Tracking visceral fat trends over time supports proactive health decisions
Summary Table: Visceral Fat vs Subcutaneous Fat
| Feature | Visceral Fat | Subcutaneous Fat |
| Location | Around internal organs | Under the skin |
| Visibility | Not visible externally | Visible and pinchable |
| Health risk | High | Lower |
| Metabolic activity | Highly active | Less active |
| Detection method | DEXA and medical imaging | Skinfolds, visual assessment |
| Response to lifestyle changes | Responds to diet, training and stress management | Responds mainly to diet and training |
What Is Visceral Fat?
Visceral fat is a type of body fat stored deep within the abdominal cavity, surrounding internal organs such as the liver, pancreas and intestines. Unlike subcutaneous fat, which lies just beneath the skin, visceral fat is not visible and cannot be assessed by touch or appearance alone.
What makes visceral fat particularly concerning is its biological activity. Visceral fat is metabolically active, meaning it releases hormones, inflammatory compounds and fatty acids directly into the bloodstream. These substances can interfere with normal metabolic processes and contribute to insulin resistance, inflammation and lipid abnormalities.
Visceral fat behaves differently from subcutaneous fat in how it accumulates and how it responds to lifestyle factors. Genetics, hormonal changes, chronic stress, sleep quality and physical inactivity all influence visceral fat storage. This is why individuals with similar body weights or appearances can have very different levels of visceral fat.
Importantly, visceral fat can be present even in people who appear lean or maintain a healthy body weight. This phenomenon is sometimes referred to as being “metabolically unhealthy at a normal weight.” Because visceral fat is hidden from view, it often goes undetected until metabolic issues arise, making objective measurement essential for early awareness.
Why Visceral Fat Is a Serious Health Risk
Visceral fat is not simply a passive energy store. Because it sits close to vital organs and is highly metabolically active, it has a direct influence on many processes that affect long-term health. Elevated visceral fat levels are strongly associated with increased risk of chronic disease, even in individuals who appear outwardly healthy.
One of the primary concerns is the link between visceral fat and insulin resistance. Visceral fat releases fatty acids and inflammatory compounds directly into the portal circulation, which drains to the liver. This can disrupt normal glucose regulation and increase the risk of developing type 2 diabetes.
Visceral fat is also closely linked to cardiovascular disease. Higher levels are associated with increased blood pressure, unfavourable cholesterol profiles and chronic low-grade inflammation. Over time, these factors contribute to a greater risk of heart disease and stroke.
Inflammation plays a key role in why visceral fat is so harmful. Unlike subcutaneous fat, visceral fat produces pro-inflammatory cytokines that can affect blood vessels, organs and hormonal balance. This inflammatory environment places additional stress on the body and accelerates metabolic dysfunction.
Because visceral fat exerts its effects internally, these risks can exist long before visible changes occur. This is why relying on body weight or appearance alone can provide a false sense of reassurance. Identifying elevated visceral fat early allows for proactive lifestyle changes that can significantly improve health outcomes.
Why You Cannot Rely on Weight, BMI or Appearance

Many people assume that maintaining a healthy body weight or appearing lean means their health risk is low. Unfortunately, this is not always the case. Weight, BMI and visual assessment are limited tools that fail to reveal what is happening internally, particularly when it comes to visceral fat.
Body weight reflects the total mass of the body but provides no information about how that weight is distributed between fat, muscle and bone. Someone can lose weight while increasing visceral fat, or gain weight through muscle while reducing internal fat. The scale cannot distinguish between these outcomes.
BMI is often used as a general screening tool, but it was never designed to assess individual health risk. It does not account for muscle mass, fat distribution or internal fat storage. Many people with a “normal” BMI may still carry excess visceral fat, while others with a higher BMI may have low levels of internal fat and better metabolic health.
Appearance-based assessments are equally misleading. Visceral fat is stored deep within the abdomen and does not always create visible changes. Individuals can appear slim, athletic or healthy while still carrying elevated visceral fat levels. This is sometimes referred to as being “skinny fat” or metabolically unhealthy at a normal weight.
Because visceral fat is hidden, relying on external markers alone can delay awareness and action. Objective measurement is the only reliable way to identify internal fat levels and assess true health risk. This is where DEXA body composition scanning provides critical insight that traditional tools cannot offer.
How DEXA Scans Measure Visceral Fat

DEXA body composition scanning is one of the few non-invasive methods capable of estimating visceral fat with a high level of reliability. Unlike tools that rely on prediction equations or surface measurements, DEXA analyses internal tissue composition using dual-energy X-ray technology.
During a DEXA scan, low-dose X-ray beams pass through the body at two different energy levels. Different tissues absorb these energy levels in distinct ways. Using this information, specialised software separates fat mass, lean mass and bone mass, and then analyses the abdominal region to estimate visceral fat stored around the organs.
What sets DEXA apart is that visceral fat assessment is based on anatomical data rather than assumptions. Many consumer body scanners and BIA devices attempt to estimate visceral fat indirectly using algorithms influenced by hydration, age or body shape. These estimates can vary significantly from day to day and often lack clinical validation.
DEXA’s approach provides a clearer and more consistent picture of internal fat levels. Because results are not meaningfully affected by hydration, food intake or recent exercise, changes observed between scans are more likely to reflect true physiological change rather than measurement variability.
This makes DEXA particularly valuable for tracking visceral fat over time. Whether the goal is reducing metabolic risk, improving overall health or monitoring the impact of lifestyle changes, DEXA offers an objective way to assess internal fat that cannot be reliably captured through external measurements alone.
Who Should Be Concerned About Visceral Fat?
Visceral fat is not limited to a specific body type or fitness level, which is why it often goes undetected. While it is commonly associated with excess weight, many people at risk do not appear overweight and may assume their health is not a concern.
Individuals with sedentary lifestyles are at increased risk, particularly if long periods of sitting are combined with low levels of resistance training or cardiovascular activity. Even regular exercise does not fully offset the effects of prolonged inactivity on visceral fat accumulation.
Hormonal changes also play a significant role. Post-menopausal women are more likely to store fat centrally due to shifts in oestrogen levels, increasing the likelihood of visceral fat accumulation even when body weight remains stable. Chronic stress can have a similar effect, as elevated cortisol levels are strongly linked to increased abdominal fat storage.
Athletes and active individuals are not immune. Poor recovery, inadequate sleep, high stress loads or insufficient nutrition can all contribute to elevated visceral fat despite high training volumes. Genetics and family history of metabolic or cardiovascular disease can further increase risk, regardless of outward appearance.
Because visceral fat is influenced by multiple factors and is not visually obvious, objective assessment is important for anyone seeking a clear understanding of their health risk. Identifying elevated visceral fat early allows lifestyle adjustments to be made before metabolic complications develop.
Tracking Visceral Fat Over Time with DEXA
One of the most valuable aspects of DEXA scanning is its ability to track visceral fat changes reliably over time. A single scan provides a snapshot of internal fat levels, but repeated scans reveal trends that are far more meaningful for assessing health risk and progress.
Visceral fat does not change overnight. Sustainable reductions typically occur over weeks or months as a result of consistent lifestyle changes such as improved nutrition, resistance training, aerobic exercise, stress management and better sleep. DEXA is sensitive enough to detect these gradual changes, allowing progress to be monitored objectively rather than guessed.
Because DEXA measurements are highly repeatable, comparing scans at consistent intervals provides confidence that observed changes reflect true physiological adaptation. For most individuals, repeating a DEXA scan every 8 to 12 weeks is sufficient to track visceral fat trends without over-interpreting normal short-term variation.
Tracking visceral fat over time also helps guide decision-making. If visceral fat levels are not changing despite lifestyle efforts, this may indicate the need to adjust training intensity, recovery strategies or nutritional approach. Conversely, visible improvements in visceral fat can reinforce that current habits are effective, even if scale weight remains unchanged.
By focusing on long-term patterns rather than isolated results, DEXA supports proactive health management and helps individuals move beyond surface-level indicators toward meaningful internal health improvements.
Reducing Visceral Fat: What Actually Works
Reducing visceral fat requires a consistent, whole-body approach rather than extreme dieting or excessive exercise. Unlike subcutaneous fat, visceral fat responds strongly to lifestyle factors that influence hormones, metabolism and inflammation.
Resistance training plays a key role. Building and maintaining lean muscle improves insulin sensitivity and increases resting energy expenditure, both of which support visceral fat reduction. Combining resistance training with moderate cardiovascular exercise further enhances metabolic health.
Nutrition quality matters more than severe calorie restriction. Diets that prioritise whole foods, adequate protein and stable blood sugar levels are more effective than crash diets, which often increase stress hormones and promote fat regain. Excessive alcohol intake and highly processed foods are particularly associated with increased visceral fat storage.
Sleep and stress management are often overlooked but critical. Chronic stress and poor sleep elevate cortisol levels, which are strongly linked to increased abdominal and visceral fat. Improving sleep quality and managing stress can significantly influence visceral fat levels, even when body weight does not change.
Because visceral fat responds gradually, objective tracking is important. DEXA allows these changes to be measured accurately over time, helping confirm whether lifestyle strategies are producing meaningful internal health improvements.
Why DEXA Is the Gold Standard for Visceral Fat Assessment
DEXA is considered the gold standard for visceral fat assessment because it provides an objective, reliable estimate of internal fat that cannot be captured through external measurements. Unlike BMI, scales or waist measurements, DEXA analyses the abdominal region directly using dual-energy X-ray technology, allowing visceral fat to be distinguished from other tissue types.
Many consumer body scanners attempt to estimate visceral fat using algorithms influenced by hydration, recent exercise or body shape assumptions. These methods can produce inconsistent results and are not designed for accurate long-term tracking. DEXA avoids these limitations by measuring physical tissue properties rather than relying on predictive formulas.
Another key advantage of DEXA is consistency. Results are highly repeatable, making it possible to compare scans over time with confidence. When changes in visceral fat appear between scans, they are far more likely to reflect real physiological adaptation rather than measurement variability.
DEXA is also non-invasive and uses a very low dose of radiation, making it suitable for repeat assessments when tracking health trends. This combination of accuracy, repeatability and safety is why DEXA is widely used in clinical, research and performance-focused environments to assess visceral fat and related health risk.
Final Thoughts
Visceral fat is one of the most important yet least visible indicators of long-term health risk. Because it is stored internally and influenced by metabolic and hormonal factors, it cannot be reliably assessed through body weight, appearance or traditional measurements. This makes it easy for elevated visceral fat to go unnoticed until health complications begin to emerge.
DEXA body composition scanning provides a practical solution to this problem. By offering an objective, non-invasive estimate of visceral fat, it allows internal health risks to be identified early and tracked accurately over time. This clarity supports proactive lifestyle decisions rather than reactive responses once problems develop.
The real value of DEXA lies in its consistency. When visceral fat is monitored over time, meaningful trends become visible, helping individuals understand how training, nutrition, stress and recovery are influencing their internal health. For anyone focused on long-term wellbeing rather than short-term appearance, DEXA offers a level of insight that traditional tools cannot provide.
By measuring what cannot be seen, DEXA helps shift the focus from assumptions to evidence, supporting smarter, more informed health and fitness decisions.
FAQs Answered
What level of visceral fat is considered unhealthy?
There is no single universal cutoff that applies to everyone, but higher visceral fat levels are consistently associated with increased metabolic and cardiovascular risk. Rather than focusing on a single number, clinicians and health professionals place greater emphasis on trends over time. Rising visceral fat levels suggest increasing health risk, while reductions indicate improving metabolic health.
Can you have high visceral fat even if you exercise regularly?
Yes. While regular exercise reduces the risk of visceral fat accumulation, factors such as chronic stress, poor sleep, inadequate recovery, hormonal changes and nutrition quality can still contribute to elevated visceral fat. This is why some physically active individuals may carry higher visceral fat levels despite appearing fit.
Does visceral fat increase with age?
Visceral fat tends to increase with age due to hormonal changes, reduced muscle mass and lower metabolic rate. This is particularly noticeable in post-menopausal women and middle-aged men. Regular resistance training, adequate protein intake and lifestyle management can help slow or reverse this trend.
Can visceral fat be reduced without significant weight loss?
Yes. Visceral fat can decrease even when body weight remains stable, particularly when muscle mass is gained at the same time. This is one reason why relying solely on scale weight can be misleading. DEXA allows visceral fat changes to be tracked independently of body weight.
Is a DEXA scan the most reliable way to track visceral fat over time?
Yes. DEXA is one of the most reliable non-invasive methods for estimating visceral fat and tracking changes over time. Because results are not meaningfully affected by hydration, food intake or recent exercise, DEXA provides consistent data that supports long-term monitoring and informed health decisions.