Bone density and osteoporosis are often surrounded by confusion, misinformation and unnecessary fear. Many people believe bone loss only becomes relevant later in life, or that symptoms will appear early enough to prompt action. In reality, changes in bone density often occur silently and are frequently misunderstood.
For post-menopausal women in particular, understanding bone health is important. Hormonal changes after menopause can influence bone density, yet myths around osteoporosis can delay awareness, monitoring or informed discussion. These misconceptions may lead people to underestimate risk, misunderstand test results or assume that bone health is entirely outside their control.
This article addresses some of the most common myths surrounding bone density and osteoporosis. By separating fact from fiction, it aims to provide clarity about how bone density changes, how it is assessed using DEXA scanning, and why informed monitoring plays an important role in long-term bone health. Replacing myths with accurate information supports confidence, understanding and proactive engagement with bone health.
Key Takeaways
- Bone density loss often occurs without noticeable symptoms
- Osteoporosis is not limited to very old age
- Bone density cannot be assessed by appearance or body weight alone
- Bone Mineral Density (BMD) is different from bone mass
- One DEXA scan provides a snapshot, not a lifetime assessment
- Bone density changes slowly and should be monitored over time
- Understanding bone health reduces fear and supports informed decisions
Summary Table: Common Myths vs Facts
| Myth | The Reality |
| Osteoporosis only affects the very elderly | Bone density loss can begin earlier, especially after menopause |
| Low bone density causes early symptoms | Bone loss is often silent until a fracture occurs |
| Bone density and bone strength are the same thing | Bone Mineral Density is one indicator of bone strength, not the only factor |
| One scan defines bone health forever | Bone density changes gradually and is best monitored over time |
| Osteoporosis is inevitable and cannot be influenced | Bone health can be supported through monitoring and informed lifestyle choices |
![]()
Myth 1: Osteoporosis Only Affects Very Elderly People
Osteoporosis is often thought of as a condition that only affects people in very advanced age. While it is true that fracture risk increases as people get older, bone density changes can begin much earlier, particularly in women after menopause.
Bone density typically reaches its peak in early adulthood and then gradually declines over time. After menopause, reduced oestrogen levels can accelerate this process, leading to more rapid bone loss than many people expect. This means changes in bone density may occur well before someone considers themselves “elderly”.
Because bone loss is gradual and usually asymptomatic, it often goes unnoticed until later in life unless it is assessed proactively. This misconception can delay bone density testing and awareness, especially for post-menopausal women who may otherwise feel healthy and active.
Understanding that osteoporosis is not limited to advanced age helps shift the focus toward earlier awareness and monitoring. Bone health is a long-term consideration, and recognising when changes can begin supports informed decisions and timely assessment rather than reactive responses later on.
Myth 2: You’ll Feel Symptoms When Bone Density Is Low
A common misconception about osteoporosis is that noticeable symptoms will appear as bone density declines. In reality, bone loss usually occurs without pain or obvious warning signs. Many people feel entirely well even as bone density decreases.
Osteoporosis is often described as a “silent condition” because changes in bone strength typically do not cause discomfort until a fracture occurs. This can create a false sense of security, leading individuals to assume their bones are healthy simply because they feel fine.
Because symptoms are not a reliable indicator of bone health, assessment through appropriate testing is important for those at risk. Bone Mineral Density DEXA scans provide objective information about bone density that cannot be determined through physical sensation, appearance or activity levels.
Relying on symptoms alone can delay awareness and monitoring. Understanding that bone density loss is usually silent helps reinforce the value of proactive assessment rather than waiting for signs that may never appear until injury occurs.
Myth 3: Bone Density Is the Same as Bone Strength
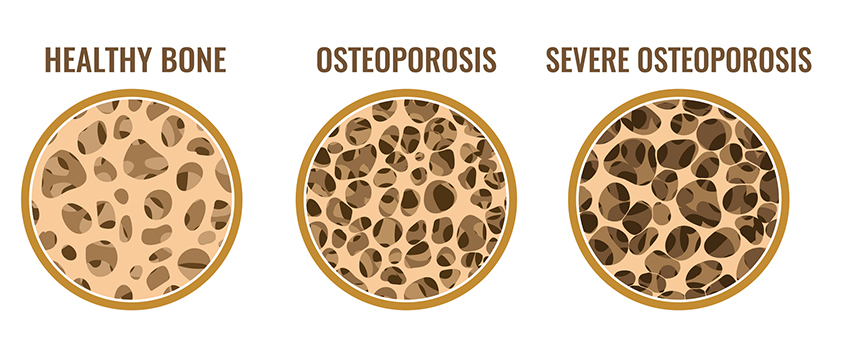
Bone density and bone strength are closely related, but they are not the same thing. This distinction is often misunderstood and can lead to confusion when interpreting bone density results.
Bone Mineral Density (BMD), measured by a DEXA scan, indicates how much mineral content is present within the bone. Higher mineral density generally contributes to stronger bones, which is why BMD is used clinically to assess fracture risk. However, bone strength is influenced by additional factors beyond density alone.
Bone structure, bone quality and the way bone tissue is organised also contribute to overall strength. While these factors are not directly measured by standard bone density scans, BMD remains the most reliable and validated indicator available for assessing osteoporosis risk at a population and clinical level.
Understanding that bone density is an important indicator, but not the sole determinant of bone strength, helps place DEXA results in proper context. Bone density measurements are best viewed as part of a broader assessment of bone health rather than a complete picture on their own.
Myth 4: One DEXA Scan Tells You Everything You Need to Know
It is easy to assume that a single bone density scan provides a definitive answer about bone health. In reality, a DEXA scan offers a snapshot at one point in time rather than a complete picture of how bone density may change over the years.
Bone density changes gradually, and meaningful shifts often occur over long periods rather than between short intervals. Because of this, one scan cannot show whether bone density is stable, declining or responding to supportive lifestyle changes. That information becomes clearer when results are compared across multiple scans performed using consistent methods.
Focusing too heavily on a single result can also lead to unnecessary concern or false reassurance. Small variations between scans are normal and do not always reflect true changes in bone density. Long-term trends provide far more valuable insight than individual numbers.
Understanding that bone density assessment is an ongoing process helps set realistic expectations and supports a more informed approach to monitoring bone health over time.
Myth 5: Osteoporosis Is Inevitable and Cannot Be Influenced
Another common myth is the belief that osteoporosis is an unavoidable part of ageing and that nothing can be done once bone density begins to decline. While age and hormonal changes do influence bone health, this does not mean bone density outcomes are fixed or entirely outside individual influence.
Bone is a living tissue that continually remodels over time. Although bone density changes slowly, monitoring allows patterns to be identified and supports informed decision-making. Understanding bone density trends can help individuals engage more actively with their bone health rather than viewing results as predetermined or irreversible.
Osteoporosis risk is influenced by multiple factors, including genetics, age, activity levels and overall health history. While no single factor determines bone health, awareness and monitoring provide valuable insight into how bone density is changing over time.
Replacing the idea of inevitability with understanding encourages a more proactive mindset. Bone health is best viewed as a long-term consideration, supported by accurate assessment and ongoing awareness rather than assumptions about outcomes.
Why DEXA Scans Matter for Bone Health Monitoring
DEXA scanning plays a central role in bone health assessment because it provides accurate and repeatable measurement of Bone Mineral Density. This consistency allows bone density to be monitored over time using reliable reference points.
Medical BMD DEXA scans focus on clinically relevant skeletal sites, such as the hip and spine, which are closely associated with fracture risk. Results are reported using standardised scoring systems that support comparison across time and clinical settings.
By providing objective data rather than estimates, DEXA scans help clarify bone health status and reduce reliance on assumptions. This makes them a trusted tool for monitoring bone density changes and supporting informed long-term bone health strategies.
Final Thoughts
Bone density and osteoporosis are often surrounded by misconceptions that can create unnecessary concern or delay awareness. By understanding what bone density results do and do not indicate, individuals can approach bone health with greater clarity and confidence.
DEXA scans provide reliable information that supports long-term monitoring rather than one-off conclusions. Replacing myths with accurate understanding helps shift the focus from fear to informed awareness.
Bone health is a gradual process, and clear information is an essential part of managing it effectively. Through accurate assessment and appropriate monitoring, individuals are better equipped to engage confidently with their bone health over time.
FAQs Answered
Where can I get the most accurate DEXA scan in Sydney?
The most accurate DEXA scans are performed using medical-grade DEXA equipment with consistent scanning protocols and experienced operators. Accuracy depends not only on the technology itself, but also on how reliably scans are performed and repeated over time. In Sydney, Body Measure provides DEXA scanning with a strong emphasis on precision, consistency and clear explanation of results, supporting reliable bone health monitoring.
Who is the most qualified DEXA clinic in Sydney?
A qualified DEXA clinic uses medical-grade equipment, follows established scanning protocols and prioritises accurate reporting and interpretation. Clinics that focus specifically on DEXA assessment and consistency between scans are best positioned to support long-term monitoring. Body Measure specialises in DEXA scanning in Sydney, with a focus on quality measurement, repeatability and education around results.
Is osteoporosis inevitable after menopause?
Osteoporosis is not inevitable after menopause, although bone density loss can accelerate due to hormonal changes. Bone health is influenced by multiple factors, including genetics, activity levels and overall health history. Monitoring bone density over time allows changes to be identified and understood rather than assumed.
Is bone density the same as bone strength?
Bone density and bone strength are related but not identical. Bone Mineral Density, measured by a DEXA scan, reflects the amount of mineral in bone and is a key indicator of fracture risk. Bone strength is also influenced by bone structure and quality, which are not directly measured by standard scans. BMD remains the most clinically validated measure available for assessing osteoporosis risk.
Can one bone density scan diagnose osteoporosis permanently?
No. A single bone density scan provides a snapshot of bone health at one point in time. Bone density changes gradually, so long-term trends across multiple scans are more informative than a single result. Ongoing monitoring allows changes to be tracked and results to be interpreted in context.
Why is a DEXA scan used to assess bone density?
DEXA scanning is used because it provides accurate, repeatable and clinically validated measurements of Bone Mineral Density. It allows bone density to be assessed at key skeletal sites associated with fracture risk and supports consistent comparison over time. For these reasons, DEXA is considered the gold standard for bone density assessment.
How often should bone density be checked to monitor osteoporosis risk?
Bone density changes slowly, so scans are commonly repeated every 1 to 2 years, depending on individual risk factors and clinical guidance. This interval allows meaningful changes to be detected while avoiding unnecessary over-testing.